News

23 May 2023
A niche for cancer
Stowers scientists are unraveling the mechanisms governing cancer stem cells
Read Article
News
Investigating how metabolism works in humans and other species may yield answers for controlling and one day even curing diabetes.

Cavefish are studied to unlock new knowledge surrounding metabolic conditions.
Five questions about diabetes
Foundational biological research conducted by scientists at the Stowers Institute for Medical Research is furthering our understanding of metabolism and metabolic diseases including diabetes. The prevalence of diabetes has risen dramatically over the past several decades, affecting 10% of the global population. The World Health Organization attributes diabetes as a major factor causing blindness, kidney failure, heart attack, stroke, and lower limb amputation. Learn more about this disease and how research from the Stowers Institute could one day help provide better avenues for treatment and potentially prevention below.
How is diabetes diagnosed and monitored?
We consume food and then our body breaks it down, or metabolizes it, into usable energy. Sugar is broken down into glucose, the primary source of fuel our cells need to function. Glucose is necessary for life but can turn toxic when not regulated properly. A hallmark of diabetes is a lack of control of glucose levels in the blood.

Blood glucose requires a hormone, insulin, produced by cells of the pancreas to transport this food breakdown product into cells. When insulin production stops or the body doesn’t respond to insulin efficiently, diabetes is diagnosed by elevated blood glucose concentrations. Monitoring blood glucose levels often involves pricking a finger and depositing a drop of blood into a machine that measures glucose concentrations.
There are three types: What is the difference?
Type 1 diabetes is considered an autoimmune disorder with a sudden onset when the pancreas simply stops making insulin. Approximately 5-10% of people living with diabetes have Type 1 and, while generally diagnosed in children and young adults, onset can occur at any age. Patients must carefully manage the condition with artificial insulin and strict multi-daily monitoring of blood glucose.
Type 2 diabetes is the most common form, accounting for over 90% of all cases. Rather than not producing insulin, the body doesn’t utilize insulin properly. Typically diagnosed later in life, disease onset is more gradual. Genetics can predispose people to developing Type 2, but lifestyle choices seem to play an equally important role in a diagnosis. If you are predisposed to Type 2 diabetes, there are measures you can take with regards to diet, exercise, and weight control to prevent the disease and at the very least delay onset.
Gestational diabetes occurs in about 7% of pregnancies. Because this condition can lead to pregnancy complications for both mom and baby, prenatal screening is standard practice. While gestational diabetes typically resolves after birth, there is an increased likelihood for women and their babies diagnosed with the condition to develop Type 2 diabetes, and regular screening is advised.

Morphological differences between surface fish with cavefish from the Pachón caves. Cavefish have evolved a feasting and fasting cycle, allowing them to store impressive amounts of body fat and starve for months with ease. Scientists at the Institute have developed a system to compare fish from the river to the fish who live in caves. It gives scientists a rare look at what happens when species adapt to extreme nutritional challenges.
How do diet and lifestyle impact diabetes?
Sedentary lifestyles, obesity, and diet are all implicated in the likelihood of developing Type 2 diabetes, particularly as inactivity, obesity, and diabetes are rising worldwide. However, research has identified many regions of genetic variations that are correlated. Regular exercise, weight control, and eating a healthy plant-forward diet low in refined sugars and alcohol are the most effective ways to reduce the chance of a diagnosis.
Multiple genes are implicated in Type 1 diabetes although the genetic basis is not fully understood. Diet and lifestyle do not seem to play a part in developing the disease—there is a nature vs nurture aspect for most autoimmune disorders, complicating the ability to predict those at risk. However, diet and lifestyle are extremely important in managing Type 1, along with life-long insulin medication. Exercise, while beneficial for many aspects of health, is more complicated and requires a careful balance of insulin, food intake, and monitoring blood glucose levels. This balance is imperative to maintain levels within a relatively narrow range to avoid complications like seizures associated with low blood sugar, or hypoglycemia.
What is the outlook on a cure for diabetes?
There is currently no cure for diabetes. As a chronic condition, it can be managed with medication and healthy lifestyle choices. For most people prone to diabetes (Type 2), the best cure is prevention.
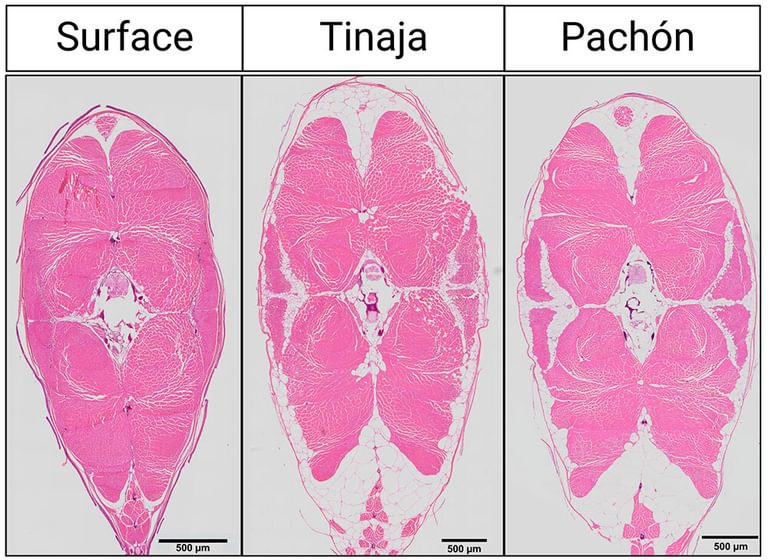
Cross section of muscle cells for surface fish and cavefish from the Pachón and Tinaja caves. Muscle fibers are depicted in pink and fat deposits are in white.
For some patients with Type 1 diabetes that is difficult to control with standard insulin treatments, ongoing clinical research is geared toward improving outcomes for pancreas or islet cell transplants (pancreatic cells from an organ donor are transplanted into the liver). All transplantation treatments come with risks of complications including immunosuppression and rejection and are still only considered for severe cases.
How can foundational research help?
Certain species like cavefish and nectar bats have evolved to consume and store large amounts of sugar. While displaying traits associated with diabetes like high blood glucose, insulin resistance, and increased fat storage, genetic adaptations allow them to remain healthy when these same traits in humans result in disease. Former Stowers Associate Investigator Nicolas Rohner, Ph.D., investigated the mechanisms underlying how these organisms cope with high blood sugar without corresponding pathologies. Some mechanisms identified so far include genetic adaptations and metabolic reprogramming.
More broadly, a key research focus of the lab of Stowers Investigator Jerry Workman, Ph.D., is how gene activity is impacted by the breakdown products of metabolism. This research may inform our understanding of normal metabolic processes as well as metabolic diseases like diabetes.
Investigating how metabolism works in humans and other species may yield answers for controlling and one day even curing diabetes.
News

23 May 2023
Stowers scientists are unraveling the mechanisms governing cancer stem cells
Read Article
News

24 April 2023
Foundational research at the Stowers Institute is leading to a greater understanding of many factors governing infertility with the goal of improving health, healthy outcomes, and providing hope for people facing this challenge.
Read Article
News

14 March 2023
Memories of “firsts”—a first kiss, first love, first heartbreak—feel permanent. But why do we remember some moments yet forget others?
Read Article
Press Release
12 May 2022
New research examines how cavefish developed unique metabolic adaptations to survive in nutrient-scarce environments.
Read Article
